Triglyceride Metabolism: Structure, Regulation, and Role in Metabolic Diseases
Triglycerides play a pivotal role in energy storage and lipid metabolism, acting as a major source of energy for the body. However, the complexities of triglyceride metabolism extend beyond energy production, influencing various aspects of health, including obesity, diabetes, cardiovascular diseases, and fatty liver disease. This comprehensive guide delves into the intricate mechanisms of triglyceride metabolism, exploring how it is regulated at the molecular, cellular, and organ levels. By understanding these regulatory processes, we can better appreciate the role of triglycerides in health and disease, and how they are measured and analyzed using advanced techniques such as gas chromatography, high-performance liquid chromatography, and mass spectrometry. Join us as we unravel the critical pathways and factors that govern triglyceride metabolism and its implications for metabolic health.
1.Structure and Chemical Properties of Triglycerides
Composition of Triglyceride Molecules
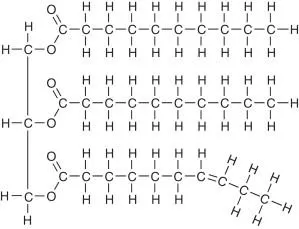
Triglycerides, also known as triacylglycerols, are the most common form of fat found in the human body and the primary form of storage for energy in the form of lipids. A triglyceride molecule is composed of one glycerol backbone attached to three fatty acids. This simple yet highly effective structure allows for the efficient storage and release of energy.
The glycerol part of a triglyceride is a three-carbon molecule that acts as a framework to which the fatty acids are attached. The fatty acids, on the other hand, are long hydrocarbon chains that can vary in length and degree of saturation. This variability in the fatty acid composition influences the physical and chemical properties of triglycerides.
Fatty acids can be saturated, meaning they have no double bonds between the carbon atoms, or unsaturated, containing one or more double bonds. Saturated fatty acids tend to be solid at room temperature, while unsaturated fatty acids are typically liquid. The balance of these types of fatty acids in a triglyceride impacts its functionality in metabolic processes and its behavior under different physiological conditions.
Importance in Lipid Metabolism
Triglycerides play a crucial role in lipid metabolism, serving as the primary storage form of energy in the body. They are stored in adipose tissue and can be mobilized when energy is required. This process is essential for maintaining energy homeostasis, particularly during periods of fasting or intense physical activity.
In the metabolic pathway, triglycerides undergo hydrolysis by lipases to release free fatty acids and glycerol. These components are then transported through the bloodstream to various tissues where they are used for energy production. Free fatty acids can enter the mitochondria of cells where they undergo beta-oxidation to produce ATP, the main energy currency of the cell.
The glycerol released from triglyceride breakdown can be used in gluconeogenesis, a process that generates glucose from non-carbohydrate sources, thus playing a pivotal role in maintaining blood glucose levels during periods of fasting. This versatility makes triglycerides indispensable for energy storage and supply, highlighting their importance in lipid metabolism and overall metabolic health.
For B2B customers in the biochemical and medical fields, understanding the structure and function of triglycerides is fundamental. It provides insight into various metabolic diseases, energy management in clinical settings, and the development of therapeutic interventions targeting lipid metabolism.
2.Triglyceride Metabolism Pathways
Synthesis, Degradation, and Transport of Triglycerides
Triglyceride metabolism encompasses a series of intricate pathways crucial for maintaining energy balance and lipid homeostasis in the body. The primary processes involved include the synthesis, degradation, and transport of triglycerides, each playing a pivotal role in overall metabolic health.
Synthesis of Triglycerides
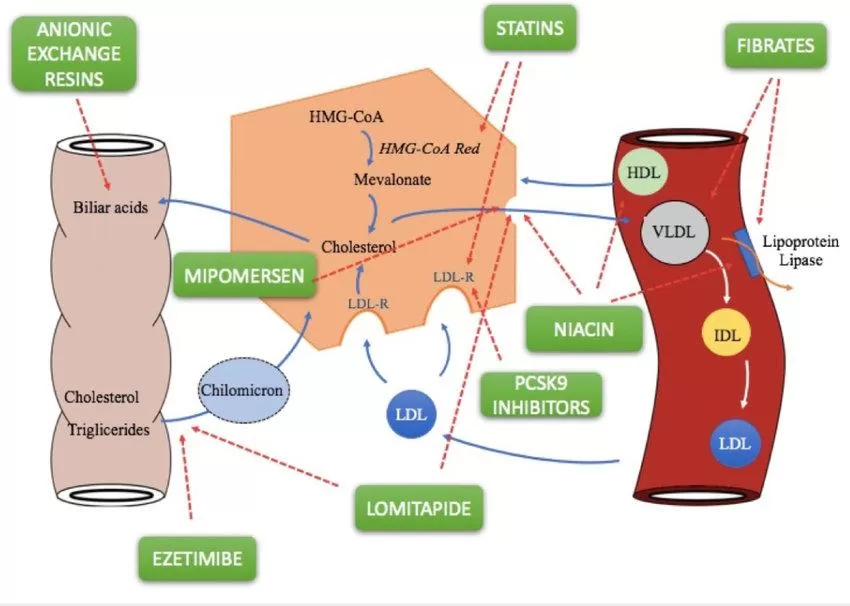
Triglyceride synthesis, or lipogenesis, predominantly occurs in the liver and adipose tissue. In the liver, excess dietary carbohydrates and proteins are converted into fatty acids through a process known as de novo lipogenesis. These fatty acids then combine with glycerol to form triglycerides. The liver packages these newly synthesized triglycerides into very low-density lipoproteins (VLDL), which are released into the bloodstream for transport to peripheral tissues where they can be stored or used for energy.
In adipose tissue, triglycerides are synthesized from glycerol and fatty acids derived from the bloodstream. These triglycerides are stored as lipid droplets, providing a crucial energy reserve that can be mobilized during periods of energy deficit or increased energy demand. This storage capability underscores the importance of adipose tissue in energy balance and lipid metabolism.
Degradation of Triglycerides
The breakdown of triglycerides, known as lipolysis, involves the hydrolysis of triglycerides into glycerol and free fatty acids. This process is primarily regulated by hormones such as glucagon and adrenaline, which trigger lipolysis during fasting or stress. The released glycerol and fatty acids are transported to various tissues, where they are utilized as energy sources, particularly during periods of prolonged physical activity or caloric restriction.
Lipolysis is a crucial metabolic process that ensures the availability of energy substrates during times of need, highlighting the dynamic nature of triglyceride metabolism in maintaining energy homeostasis. The fatty acids released can undergo beta-oxidation in mitochondria, leading to the production of ATP, the primary energy currency of the cell.
Transport of Triglycerides
Triglycerides synthesized in the liver are transported via the bloodstream in lipoprotein particles such as VLDL. These particles are crucial for delivering triglycerides to peripheral tissues, where they are either used for immediate energy needs or stored for future use. In addition to VLDL, chylomicrons, which are formed in the intestine from dietary fats, also play a significant role in triglyceride transport.
The efficient transport and delivery of triglycerides to tissues is essential for maintaining metabolic flexibility, allowing the body to adapt to varying energy demands. This process is particularly important in ensuring that tissues such as muscle and heart have a readily available source of energy, especially during periods of increased physical activity.
Key Enzymes and Regulation of Fatty Acid Synthesis and Breakdown
The metabolism of triglycerides is regulated by a complex network of enzymes and signaling pathways that control both the synthesis and breakdown of fatty acids. These enzymes play a critical role in maintaining lipid balance and ensuring that energy is efficiently stored and mobilized as needed.
Enzymes Involved in Fatty Acid Synthesis
The synthesis of fatty acids, which are the building blocks of triglycerides, involves several key enzymes. Acetyl-CoA carboxylase (ACC) is a rate-limiting enzyme that converts acetyl-CoA to malonyl-CoA, a crucial step in fatty acid synthesis. Another important enzyme, fatty acid synthase (FAS), catalyzes the subsequent reactions that lead to the formation of long-chain fatty acids.
Additionally, acyl-CoA synthetase activates fatty acids by converting them into acyl-CoA derivatives, which are then incorporated into triglycerides. The activity of these enzymes is tightly regulated by hormonal signals and nutritional status, ensuring that fatty acid synthesis is coordinated with the body's energy needs and dietary intake.
Enzymes Involved in Fatty Acid Breakdown
The breakdown of triglycerides is facilitated by enzymes such as hormone-sensitive lipase (HSL) and adipose triglyceride lipase (ATGL). HSL is activated by hormones like adrenaline and glucagon, triggering the hydrolysis of stored triglycerides into free fatty acids and glycerol. ATGL initiates the breakdown of triglycerides by hydrolyzing the first fatty acid from the glycerol backbone.
These enzymes are regulated by various factors, including hormonal signals, energy status, and intracellular mediators. For instance, during fasting or exercise, increased levels of glucagon and adrenaline promote the activation of HSL and ATGL, leading to enhanced lipolysis and the release of fatty acids for energy production.
Regulation and Impact on Metabolic Health
The regulation of triglyceride metabolism is influenced by multiple factors, including dietary intake, hormonal balance, and genetic predisposition. Dysregulation of these processes can lead to metabolic disorders such as obesity, insulin resistance, and type 2 diabetes. Understanding the pathways and regulatory mechanisms of triglyceride metabolism is crucial for developing therapeutic strategies to manage and prevent these conditions.
For businesses involved in the biochemical, pharmaceutical, and healthcare sectors, a comprehensive understanding of triglyceride metabolism is essential. It provides valuable insights into the development of treatments and interventions aimed at optimizing metabolic health and addressing lipid-related disorders.
3.Lipid Metabolism and Metabolic Diseases
Obesity and Triglycerides
Role in Fat Accumulation
Obesity is a complex metabolic condition characterized by excessive accumulation of body fat, and triglycerides play a significant role in this process. Triglycerides are the primary form of stored fat in adipose tissue. When energy intake exceeds expenditure, excess calories are converted into triglycerides and stored in adipocytes, leading to an increase in fat mass. This energy surplus and subsequent triglyceride storage are key factors in the development of obesity.
Adipocytes, or fat cells, can expand to accommodate larger amounts of triglycerides. This process, known as adipocyte hypertrophy, contributes to the increase in body fat mass. Over time, the number of adipocytes can also increase through a process called hyperplasia, further exacerbating fat accumulation. The efficiency of triglyceride storage and release from adipose tissue is regulated by various enzymes and hormones, including insulin, which promotes triglyceride synthesis and storage.
Mechanisms Linking Triglycerides and Obesity
Several mechanisms link triglycerides to obesity, primarily through their role in energy balance and lipid metabolism. Elevated levels of triglycerides in the bloodstream, often seen in obese individuals, contribute to metabolic dysregulation and increased fat storage. This dysregulation can lead to insulin resistance, a condition where the body's cells become less responsive to insulin, impairing glucose uptake and increasing blood sugar levels.
Insulin resistance further promotes triglyceride accumulation in adipose tissue by enhancing lipogenesis (fat synthesis) and inhibiting lipolysis (fat breakdown). This creates a vicious cycle where increased triglyceride storage contributes to further obesity and metabolic dysfunction. Additionally, excess triglycerides can accumulate in non-adipose tissues such as the liver and muscle, contributing to lipotoxicity and further metabolic complications.
Diabetes Mellitus
Triglyceride Metabolism in Diabetes
In diabetes mellitus, particularly type 2 diabetes, triglyceride metabolism is often disrupted, leading to elevated levels of triglycerides in the blood, known as hypertriglyceridemia. This condition is closely associated with insulin resistance and poor glycemic control. In diabetic individuals, the body's ability to regulate triglyceride synthesis and breakdown is impaired, resulting in excessive triglyceride production and reduced clearance from the bloodstream.
Insulin plays a crucial role in regulating triglyceride metabolism by promoting glucose uptake and suppressing lipolysis in adipose tissue. However, in insulin-resistant states, the suppression of lipolysis is diminished, leading to increased release of free fatty acids from adipose tissue. These fatty acids are then converted into triglycerides in the liver, contributing to elevated blood triglyceride levels and exacerbating the risk of cardiovascular disease.
Effects on Insulin Sensitivity
High levels of triglycerides and free fatty acids in the bloodstream can negatively impact insulin sensitivity, a key factor in the development of type 2 diabetes. Excess triglycerides can lead to the accumulation of lipid intermediates such as diacylglycerol and ceramides in muscle and liver cells, which interfere with insulin signaling pathways. This lipid-induced insulin resistance impairs glucose uptake by cells, contributing to elevated blood glucose levels and worsening diabetes control.
Furthermore, elevated triglycerides can promote the release of inflammatory cytokines from adipose tissue, which can further impair insulin sensitivity. This inflammation-mediated insulin resistance is a critical component of the metabolic syndrome, a cluster of conditions that increase the risk of diabetes, cardiovascular disease, and other metabolic disorders.
Cardiovascular Diseases
Triglycerides as a Risk Factor
Elevated triglyceride levels are a significant risk factor for cardiovascular diseases (CVDs), including coronary artery disease, stroke, and peripheral artery disease. High triglyceride levels contribute to the development of atherosclerosis, a condition characterized by the buildup of fatty deposits, or plaques, within the walls of arteries. This buildup narrows the arteries and restricts blood flow, increasing the risk of heart attacks and strokes.
Triglyceride-rich lipoproteins, such as VLDL, are particularly atherogenic. These particles can penetrate the arterial wall and become oxidized, triggering an inflammatory response that promotes plaque formation. The association between elevated triglycerides and cardiovascular risk is especially pronounced in individuals with other risk factors such as obesity, diabetes, and hypertension.
Mechanisms of Atherogenesis
Atherogenesis, the process of plaque formation in arteries, is closely linked to elevated levels of triglycerides and other lipid abnormalities. Triglyceride-rich lipoproteins contribute to atherogenesis through several mechanisms, including endothelial dysfunction, oxidative stress, and inflammation. These processes promote the deposition of cholesterol and other lipids within the arterial wall, leading to plaque formation and progression.
Endothelial dysfunction, a key early event in atherogenesis, is exacerbated by high triglyceride levels, which impair the ability of the endothelium to maintain vascular tone and prevent the adhesion of inflammatory cells. This dysfunction allows the penetration of lipoproteins into the arterial wall, where they undergo oxidative modification and trigger an inflammatory response, further promoting plaque development and increasing cardiovascular risk.
Fatty Liver Disease
Role of Triglycerides in Liver Health
Triglycerides play a crucial role in liver health, particularly in the context of non-alcoholic fatty liver disease (NAFLD), a common liver disorder characterized by the accumulation of excess fat in the liver. NAFLD is strongly associated with metabolic conditions such as obesity, insulin resistance, and type 2 diabetes. In NAFLD, triglycerides accumulate within hepatocytes (liver cells), leading to hepatic steatosis, or fatty liver.
The accumulation of triglycerides in the liver can impair its function and promote inflammation and fibrosis, leading to the development of non-alcoholic steatohepatitis (NASH), a more severe form of fatty liver disease. NASH can progress to liver cirrhosis and hepatocellular carcinoma, making the regulation of triglyceride metabolism critical for liver health and the prevention of liver-related diseases.
Pathogenesis of Non-Alcoholic Fatty Liver Disease (NAFLD)
The pathogenesis of NAFLD involves multiple factors, including excessive triglyceride accumulation, insulin resistance, oxidative stress, and inflammation. Insulin resistance plays a central role in the development of NAFLD by promoting increased lipolysis in adipose tissue, leading to an influx of free fatty acids to the liver. These fatty acids are then esterified to form triglycerides, resulting in hepatic steatosis.
Oxidative stress and inflammation further exacerbate liver damage by promoting lipid peroxidation, mitochondrial dysfunction, and the activation of inflammatory pathways. These processes contribute to the progression of NAFLD to NASH and the development of liver fibrosis, highlighting the importance of managing triglyceride levels and metabolic health to prevent and treat fatty liver disease.
For healthcare providers and pharmaceutical companies, understanding the mechanisms linking triglycerides to metabolic diseases is crucial for developing targeted therapies and interventions. Effective management of triglyceride levels through lifestyle changes, medications, and other therapeutic approaches can significantly reduce the risk of obesity, diabetes, cardiovascular diseases, and fatty liver disease, improving overall health outcomes.
4.Measurement and Analysis Techniques
Accurate measurement and analysis of triglyceride levels are crucial for understanding lipid metabolism and its implications for health and disease. Various advanced laboratory techniques and instruments are employed to measure triglyceride levels in biological samples, providing valuable insights into lipid profiles and metabolic conditions.
Gas Chromatography (GC)
Gas Chromatography (GC) is a powerful analytical technique widely used for separating and quantifying the components of complex mixtures, including the specific fatty acids within triglycerides. GC is particularly effective in determining the concentration of various fatty acids, providing detailed information about the fatty acid composition of triglycerides in biological samples.
The process begins with the transmethylation of triglycerides into fatty acid methyl esters (FAMEs). This conversion is essential because it allows the fatty acids to be volatilized and separated by GC based on their boiling points and polarity. The separated FAMEs are then detected using a flame ionization detector (FID), which provides high sensitivity and specificity for quantitative analysis.
GC analysis is a cornerstone in lipid research and specialized lipid profiling, offering valuable data on individual fatty acids. This information is crucial for understanding the lipid composition of various biological samples, including blood and tissue samples, which can provide insights into lipid metabolism and related health conditions.
High-Performance Liquid Chromatography (HPLC)
High-Performance Liquid Chromatography (HPLC) is another versatile and widely used technique for the analysis of triglycerides. HPLC operates by separating components in a mixture based on their interactions with a stationary phase and a mobile phase, providing high resolution and sensitivity for complex lipid mixtures.
For triglyceride analysis, the sample undergoes an extraction process to isolate triglycerides, which are then separated using an HPLC column. The detection of triglycerides can be achieved through various detectors, including ultraviolet (UV) detectors and refractive index detectors, each offering distinct advantages for lipid analysis.
HPLC's high sensitivity and precision make it a preferred choice for both research and clinical settings. It allows for the accurate identification and quantification of triglycerides in complex biological samples, facilitating studies on lipid metabolism, dietary effects on lipid levels, and the diagnosis and monitoring of lipid-related diseases.
Mass Spectrometry (MS)
Mass Spectrometry (MS) is an advanced analytical technique that provides detailed information on the molecular composition and structure of triglycerides and their constituent fatty acids. MS works by ionizing molecules and then separating the resulting ions based on their mass-to-charge ratios, offering precise mass measurements and structural insights.
In triglyceride analysis, tandem mass spectrometry (MS/MS) is often employed to identify specific fatty acids within triglyceride molecules. This technique involves multiple stages of mass analysis, allowing for the detection of specific lipid species and providing comprehensive insights into lipid metabolism and fatty acid composition.
MS methods, including liquid chromatography-mass spectrometry (LC-MS), are widely used in lipidomics research to analyze complex lipid profiles and metabolic pathways. These techniques enable the detailed characterization of lipid species, facilitating the study of lipid metabolism, biomarker discovery, and the elucidation of disease mechanisms related to lipid disorders.
Data Analysis Methods
Data analysis is a critical component of triglyceride research, involving the application of statistical and computational methods to interpret experimental results and derive meaningful conclusions. Various statistical tools are employed to analyze differences between groups, assess correlations, and visualize data trends.
Commonly used statistical methods include t-tests for comparing means between groups, ANOVA (analysis of variance) for examining differences across multiple groups, and regression analysis for exploring relationships between variables. These methods help researchers understand the impact of different factors on triglyceride levels and their associations with health outcomes.
Graphical representations, such as bar charts, line graphs, scatter plots, and heatmaps, are essential for visualizing data and trends effectively. Data visualization aids in the interpretation of complex datasets, making it easier to identify patterns and relationships that may be relevant to lipid metabolism and disease.
Advanced bioinformatics tools and software are also utilized for lipidomics data analysis, enabling the identification and characterization of specific lipid species and their roles in metabolic pathways. These tools facilitate the integration of large-scale lipid data, providing a comprehensive view of lipid metabolism and its implications for health and disease management.
For researchers and clinicians, the accurate measurement and analysis of triglycerides are crucial for advancing our understanding of lipid metabolism and developing effective strategies for the prevention and treatment of metabolic disorders. Through the application of sophisticated analytical techniques and data analysis methods, we can gain valuable insights into the complex relationships between triglycerides and health, paving the way for improved clinical outcomes and personalized therapeutic approaches.
5.Regulation Mechanisms of Triglyceride Metabolism
The regulation of triglyceride metabolism is a complex and tightly controlled process, involving multiple levels of regulation to ensure energy balance and lipid homeostasis. These mechanisms include gene expression regulation, various signaling pathways, and coordination at both cellular and organ levels. Understanding these regulatory processes is crucial for comprehending the role of triglycerides in health and disease.
Gene Expression Regulation
Gene expression regulation plays a fundamental role in controlling triglyceride metabolism. The regulation of genes involved in triglyceride synthesis, storage, and breakdown is mediated by specific transcription factors and non-coding RNAs, which modulate the transcriptional and post-transcriptional levels of these genes.
Transcription Factors in Triglyceride Metabolism
Several transcription factors are crucial in regulating the genes involved in triglyceride metabolism. These transcription factors respond to various metabolic signals and alter the expression of target genes accordingly, thus maintaining lipid homeostasis.
- SREBPs (Sterol Regulatory Element-Binding Proteins): SREBPs are key regulators of lipid biosynthesis. When cellular lipid levels are low, SREBPs are activated and translocate to the nucleus. They bind to sterol regulatory elements (SREs) in the promoters of lipid metabolism genes, upregulating the expression of genes involved in fatty acid and triglyceride synthesis, thus promoting lipid storage.
- PPARs (Peroxisome Proliferator-Activated Receptors): PPARs are a family of transcription factors that play a significant role in regulating lipid metabolism and energy homeostasis. Activated by fatty acids and their derivatives, PPARs regulate the expression of genes involved in fatty acid uptake, storage, and oxidation, thus modulating triglyceride metabolism.
Non-Coding RNAs in Triglyceride Metabolism
Non-coding RNAs, including microRNAs (miRNAs) and long non-coding RNAs (lncRNAs), also contribute to the regulation of triglyceride metabolism by modulating gene expression at the post-transcriptional level.
- miRNAs: miRNAs are small RNAs that can target specific mRNAs, leading to their degradation or inhibition of translation. Certain miRNAs are involved in the regulation of genes associated with lipid metabolism, influencing processes such as lipogenesis and lipolysis.
- lncRNAs: lncRNAs function in gene regulation by interacting with chromatin-modifying proteins and transcription factors. Some lncRNAs are implicated in the regulation of lipid metabolism pathways, thereby affecting triglyceride levels and metabolism.
Signaling Pathways in Triglyceride Metabolism
Signaling pathways play a vital role in regulating triglyceride metabolism by responding to cellular and environmental cues. These pathways coordinate the synthesis, storage, and breakdown of triglycerides to match the metabolic demands of the organism.
Insulin Signaling Pathway
Insulin is a key hormone that regulates triglyceride metabolism, particularly in response to elevated blood glucose levels. Upon insulin binding to its receptor, a cascade of intracellular signaling events is triggered, promoting fatty acid and glucose uptake in adipose tissue and liver, thus enhancing triglyceride synthesis and storage.
- In adipose tissue, insulin stimulates the uptake of glucose and fatty acids, facilitating triglyceride synthesis and storage. It also inhibits lipolysis, thereby reducing the breakdown of triglycerides into free fatty acids.
- In the liver, insulin promotes the uptake of glucose and fatty acids, enhancing triglyceride synthesis and reducing fatty acid oxidation. This leads to the accumulation of triglycerides, which are then transported to peripheral tissues for energy storage.
Glucagon Signaling Pathway
Glucagon is a hormone that acts in opposition to insulin, promoting the mobilization of energy stores during fasting or low blood glucose levels. Glucagon stimulates lipolysis in adipose tissue, leading to the breakdown of triglycerides into fatty acids and glycerol, which are then released into the bloodstream for energy production in other tissues.
- In adipose tissue, glucagon activates lipolysis, increasing the release of free fatty acids and glycerol, which are used for energy production during fasting.
- In the liver, glucagon promotes the breakdown of stored glycogen into glucose and enhances gluconeogenesis, increasing fatty acid oxidation for energy production.
AMP-activated Protein Kinase (AMPK) Pathway
AMP-activated protein kinase (AMPK) is a critical regulator of cellular energy homeostasis. AMPK is activated in response to low energy levels, indicated by a high AMP/ATP ratio, and acts to restore energy balance by promoting energy-generating processes and inhibiting energy-consuming pathways.
- AMPK activation stimulates fatty acid oxidation and inhibits lipogenesis, thus promoting the utilization of stored triglycerides for energy production.
- By inhibiting lipid synthesis and promoting fatty acid oxidation, AMPK helps conserve energy and maintain cellular energy balance.
Role of Triglyceride Metabolism Regulation at the Cellular and Organ Levels
The regulation of triglyceride metabolism is crucial for maintaining lipid homeostasis at both the cellular and organ levels. Proper regulation ensures that lipid synthesis and breakdown are balanced to meet the metabolic needs of different tissues and organs.
Cellular Level
At the cellular level, triglyceride metabolism is regulated to align with the cell's energy demands and nutrient availability. Key transcription factors, such as SREBPs and PPARs, orchestrate the expression of genes involved in lipid metabolism, ensuring that triglyceride levels are adjusted according to metabolic needs.
- AMPK acts as a cellular energy sensor, adjusting triglyceride metabolism in response to changes in cellular energy status. When energy levels are low, AMPK activation promotes fatty acid oxidation and inhibits lipid synthesis to generate energy.
- Transcription factors and non-coding RNAs fine-tune gene expression to regulate the balance between lipid synthesis, storage, and breakdown, thereby maintaining lipid homeostasis within the cell.
Organ Level
At the organ level, triglyceride metabolism regulation ensures the coordinated storage and utilization of lipids across different tissues. This coordination is essential for maintaining overall energy balance and metabolic health.
- In adipose tissue, triglycerides are stored during periods of energy excess and mobilized during periods of energy demand. Insulin and glucagon regulate lipolysis and lipogenesis to control triglyceride storage and release.
- In the liver, triglycerides are synthesized from excess glucose and fatty acids, which are then transported in lipoproteins to other tissues for energy utilization. The liver also plays a critical role in lipid metabolism and cholesterol synthesis.
Conclusion: Bridging Triglyceride Metabolism and Metabolic Health with MetwareBio
Understanding the complex regulation of triglyceride metabolism is essential for addressing various metabolic diseases, including obesity, diabetes, cardiovascular conditions, and fatty liver disease. Advances in measurement and analysis techniques, such as those offered by leading proteomics and metabolomics service provider MetwareBio, enable precise and comprehensive insights into lipid metabolism. MetwareBio’s cutting-edge technology and expertise in lipidomics provide invaluable support for researchers and clinicians seeking to unravel the complexities of triglyceride metabolism. With their global presence and commitment to scientific excellence, MetwareBio stands as a trusted partner in the quest for better metabolic health. Discover how MetwareBio can support your research and clinical needs by visiting their website at https://www.metwarebio.com/.
Next-Generation Omics Solutions:
Proteomics & Metabolomics
Ready to get started? Submit your inquiry or contact us at support-global@metwarebio.com.